
Are you experiencing shoulder pain and it’s not related to Calgary’s weather? Maybe it’s frozen shoulder.
Are you finding it more difficult to move your shoulder? Is it becoming progressively more stiff and painful? Are you unable to participate in some of your daily activities because of pain and limited shoulder mobility but you cannot think of anything you have done to injure yourself?
Well, you may be suffering from a condition called Frozen Shoulder that affects up to 5% of the population. And no, it is not related to the weather.
Can you use something from the movie frozen?? Are we allowed
Other ideas – add snow or iceberg
What is Frozen Shoulder?
Frozen shoulder is a condition that commonly affects the joint of an individual’s non-dominant shoulder and causes progressive stiffening and pain that commonly lasts between 5 and 24 months. (1) It can be caused by trauma or injury to the shoulder, but it can also occur randomly without a known cause.
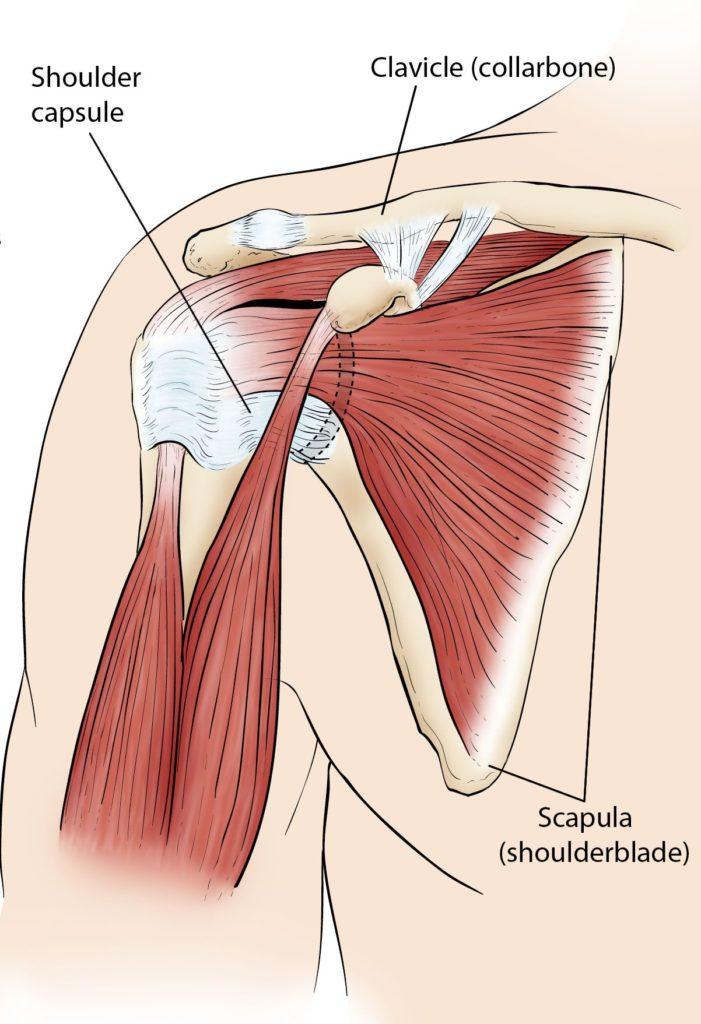
The pain and stiffness experienced with frozen shoulder is due to inflammation in the support structures that stabilize the shoulder joint. Prolonged inflammation of these structures results in their stiffening. The muscles continue working properly, however, they are unable to move the shoulder properly due to pain and stiffness in the ligaments and supportive structures. It may be helpful to think of the shoulder joint functioning like an old rubber band that has lost its elasticity.

Who gets frozen shoulder?
There are two types of frozen shoulder classifications: primary frozen shoulder and secondary frozen shoulder. Primary frozen shoulder results in a random onset of pain and stiffness without a known cause or triggering event. Secondary frozen shoulder is related to certain risk factors or may be caused by a traumatic event, surgery, or injury. (3)
There are several risk factors that increase the chances of an individual developing frozen shoulder.
Those risk factors include:
- Being age 40-65
- Having diabetes (type 1 or 2)
- Having thyroid disease
- Having a history of Dupuytren’s disease
- Being of female sex
It is important to remember that these are only risk factors and do not mean that you necessarily have frozen shoulder or will develop frozen shoulder in your lifetime.
My shoulder has been stiff and painful for months…. Is this normal?
As mentioned previously, frozen shoulder is a persistent condition and takes a significant amount of time to run its course. Without any intervention or treatment, frozen shoulder normally last between 5 and 24 months but has the possibility of lasting upwards of 3 years.
The normal progression of frozen shoulder follows 3 stages:
- The Freezing stage: the shoulder becomes gradually more stiff and painful. This stage usually lasts between 2-9 months.
- Pain at rest and with movement.
- The Frozen stage: the shoulder is at its stiffest and the pain is decreasing or absent. This stage lasts between 4-12 months.
- Only pain with movement
- The Thawing stage: the shoulder stiffness is decreasing and the pain is minimal or non-existent. This stage lasts between 5-24 months.
For the resolution of frozen shoulder, all patients are required to go through this 3-stage process, however, the severity and length of each stage is different for everyone.
Unfortunately, some patients never recover completely from frozen shoulder and will have lasting mobility issues. A physiotherapist can help determine if you are really suffering from frozen shoulder and if you are, can help prevent lifelong mobility issues and speed up your recovery process.
What are the best-known treatments for Frozen Shoulder?
When looking at the management of frozen shoulder, successful treatment is defined as a decrease in pain, and an increase in function and patient satisfaction. Due to the nature of frozen shoulder, a gradual return of a patient’s shoulder mobility is expected to occur naturally over many months.
There are many different types of treatments that have been used for frozen shoulder including physiotherapy, surgery, corticosteroid injections and pain medications. However, the “best” treatment method is still highly debated. It has been found that patients following a physiotherapy program in combination with medical management from their doctor will see the fastest resolution of symptoms and return of function, usually occurring within 6-18 months. (1,4)
What can physiotherapy do for you?
Although there is not “one best treatment option” for frozen shoulder, giving physiotherapy the cold shoulder is not the answer. At Avenue Physio, a physiotherapist will be able to:
- Assess what stage of frozen shoulder you are experiencing.
- Help you find ways to modify your activities so you can still participate in daily tasks to the best of your abilities.
- Provide manual therapy and guide you through a stretching and exercise program.
- Provide evidence informed therapeutic modalities such as Shock Wave Therapy.
- Help manage your expectations in relation to your recovery process.
- Work with your Doctor to help manage your pain and loss of function.
What can you do for yourself?
While waiting to see a physiotherapist you can take an active role in managing your own condition by: (4)
- Applying heat or ice to the affected shoulder for pain management.
- Keep the shoulder moving in a pain free range. Immobilizing the shoulder can make the condition worse. You can place objects higher at home to encourage you to lift your arm.
- Avoid sleeping on the affected side.
- Over the counter pain medication. Speak to your pharmacist or doctor about which over the counter pain medication may work best for you.
- Be patient. Frozen shoulder is a stubborn condition that takes a long time to heal, it is important to stay positive and let it run its course.
- Be conscious of your neck and back posture. Shoulder problems can often lead to neck and back problems as well, staying conscious of your posture can help avoid additional pain in these areas.
FAQ
What is the main cause of frozen shoulder?
We don’t fully understand what causes a frozen shoulder, but an inflammatory process is most likely involved. Sometimes it is caused after the shoulder has been immobilized after an injury, surgery or illness. And other times it seems to happen for no reason.
What is the fastest way to get rid of a frozen shoulder?
Sadly there does not appear to be a fast way to get rid of a frozen shoulder. Firstly you need to know what phase you are at of the normal course of a frozen shoulder: freezing, frozen or thawing. In the freezing stage the goal is to manage the pain and work on gentle ROM exercises. In the frozen stage range of motion exercise working into pain. In the thawing stage progression of range of motion exercises.
How does a frozen shoulder feel?
In the freezing stage a frozen shoulder can be quite painful and will refer to the deltoid area (the cap of your shoulder). It can be painful at night and quite sharp and debilitating with certain movements. In the frozen stage you only experience pain with movement. In the thawing stage the pain will be less and you will notice your range improving.
Come see a physiotherapist at Avenue Physio, we will give you a shoulder to cry on.

Written by Kelly Barrie
Kelly is the owner of Avenue Physio and is proud to be part of a supportive and personable team that is dedicated to providing a high quality of treatment and experience to patients. She has been a physiotherapist for over 25 years treating a range of orthopedic conditions including chronic pain, motor vehicle collisions, and sports injuries (from the weekend warrior to high level). Kelly has always been passionate about movement and promoting healthy lifestyles. First, as a Certified Personal Trainer, and for the last 25 years as a physiotherapist. Kelly has completed the highest level of Certification in Manual and Manipulative Therapy that is internationally recognized (FCAMPT). Advanced knowledge of strengthening programs, manual therapy skills, and critical thinking optimize her treatment plans for her patients so they can reach their movement goals.
