
How to best manage your birth experience
Whether it’s your first pregnancy or your fifth, giving birth can be a scary and anxiety-provoking experience. Personally, my two birth experiences were night and day! My first was a planned C section – controlled, predictable, uninvolved. My second was a vaginal birth – unpredictable, unmedicated, super involved.
Giving birth is a vulnerable place to be. Therefore, I want to share this information so that you feel empowered, informed, and in control of your next birth experience.

First, let’s take a look at the three stages of labour.
Labour is defined as work. And oh boy, are there any truer words than working to bring a baby into the world?
During labour, the cervix will “efface” or thin and begin to dilate until full dilation of 10 cm.
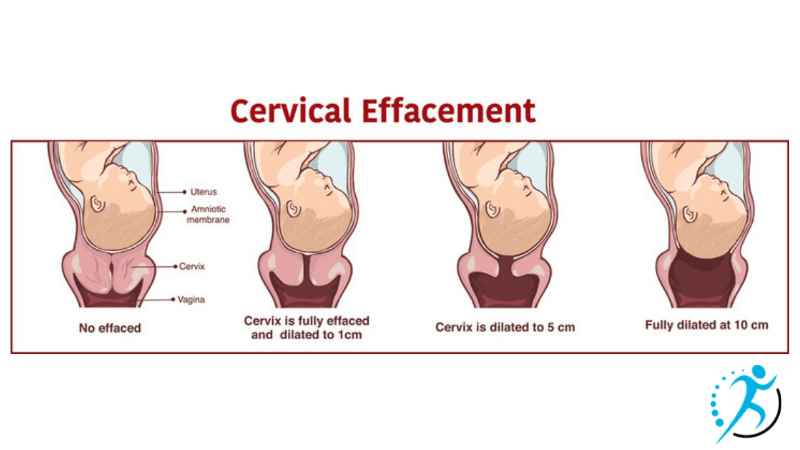
The first stage of labour has 3 phases.
Phase one (Early):
- This stage of labour can last hours if not days. Contractions are usually mild, irregular, and typically last less than 1 minute, every 5-20 minutes.
Phase two (Active):
- Contractions become stronger and more intense. Contractions in active labour occur every 2-3 minutes and last 45-75 seconds long. Warm baths and partner massage can help with coping. It is usually during this phase of labour that you should head to the hospital.
Phase 3 (Transition):
- Contractions are most intense and frequent at this stage of labour, lasting 60- 90 seconds and about 2 minutes apart. Barely any breaks! Hold on mama, you can do it! Cervical dilation is 7-10cm.
Stage 2 (Pushing phase & birth):
You are 10 cm dilated and are ready to push once you feel the urge. Sometimes there is a natural break, 20 – 30 minutes, between being fully dilated and the urge to push. Take the time to rest and recover if you can!
The pushing phase can last up to 3 hours (although, this should be absolute max!), but the typical time is 30 minutes to an hour and a half.
Research states that women should be supported in their preferred positions to push and way of breathing. That means, if it feels best to breathe (open glottis) through your contractions, then do that! And if it feels best to hold your breath (closed glottis) then do that. Do not feel pressure to push when you are coached to do so. Listen and trust your body. Do what feels right for you!
Stage 3 (Delivery of placenta):
After delivering your baby, delivery of the placenta will feel like a walk in the park. You may not even notice as most likely, you are seeing your baby for the first time and having precious skin to skin.
Now let’s review some different birth positions that you can use:
- Lithotomy: laying on your back with your legs supported or in stirrups. The historically common position of delivery. The sacrum is “fixed” against the bed, reducing the pelvic outlet.
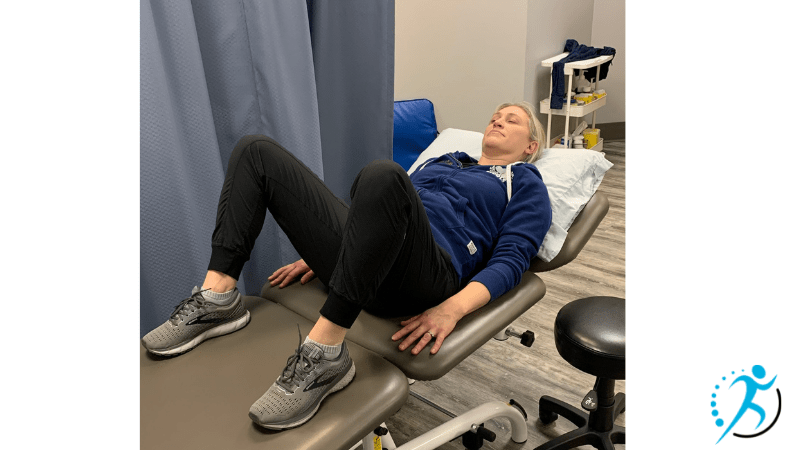
- Exaggerated Lithotomy: Hips are bent up towards armpits by holding onto legs or using stirrups. This position can facilitate a “stuck” baby out from beneath the pubic bone.
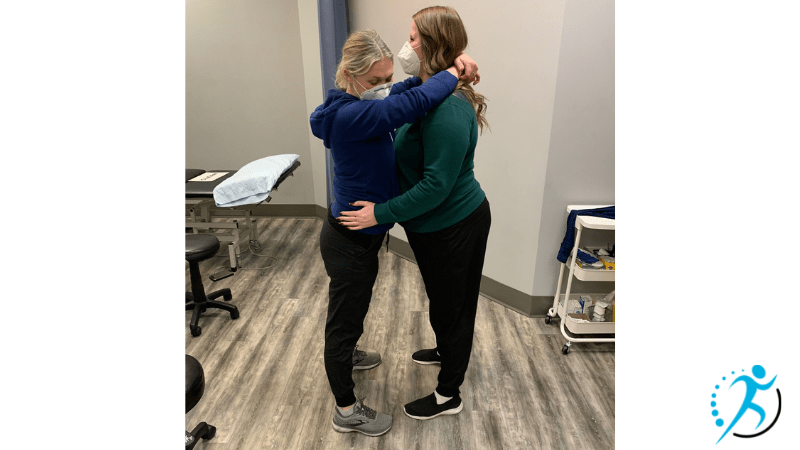
- Standing with support: Uses gravity and may assist in having the baby descend into the pelvis. Can relieve back pain.
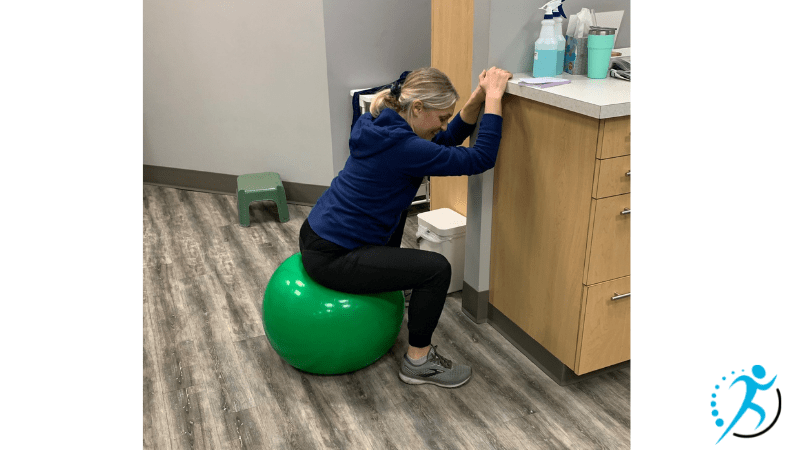
- Sitting on the ball: Can be a restful position between contractions. Helps to relax the pelvic floor and gravity helps the baby descend into the pelvis.
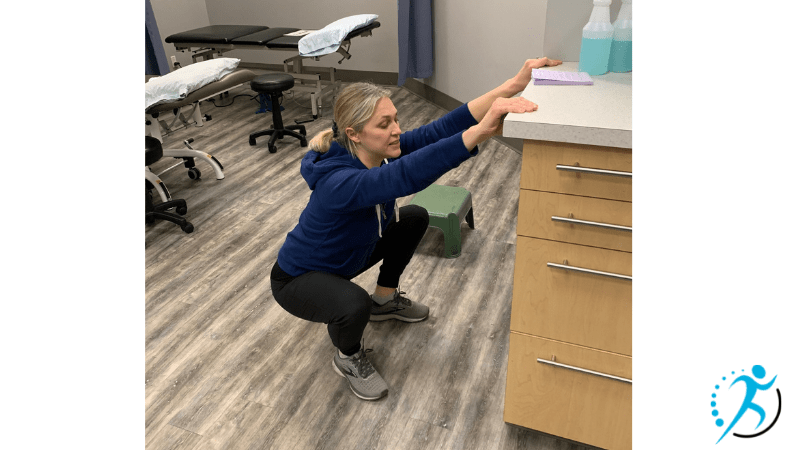
- Deep Squat with support: Uses gravity to help baby descend and opens up pelvic outlet. This position requires less bearing down effort and is still able to shift into positions of comfort. Can use hands or elbows for support.
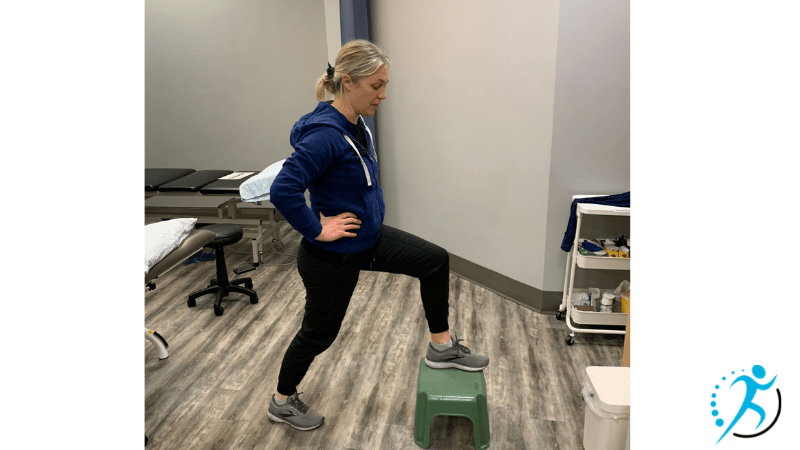
- Lunge: This position helps widen the pelvis on the side of the lunge. It can help decrease back pain & to rotate a baby if they are positioned occiput posterior (facing forward instead of inward)
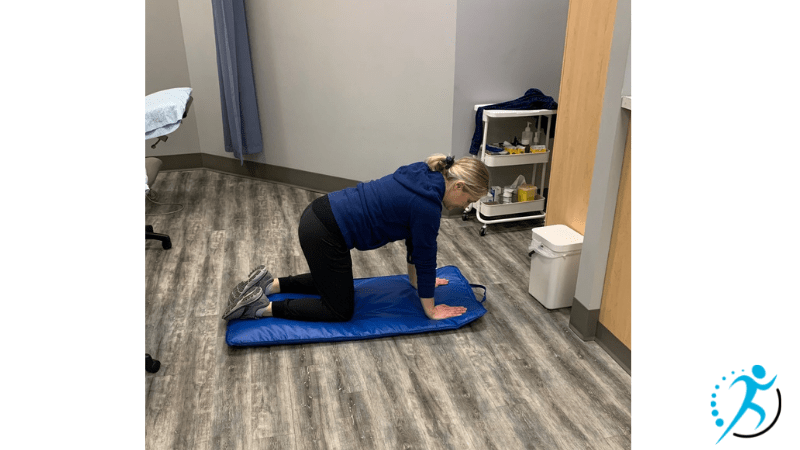
- Quadruped (hands and knees): Helps to relieve back pain. Can assist to rotate baby who is positioned occiput posterior. Can help relieve pressure from haemorrhoids and also, medical staff can still perform a vaginal exam. You can shift your body and rock back and forth to relax the pelvic floor.
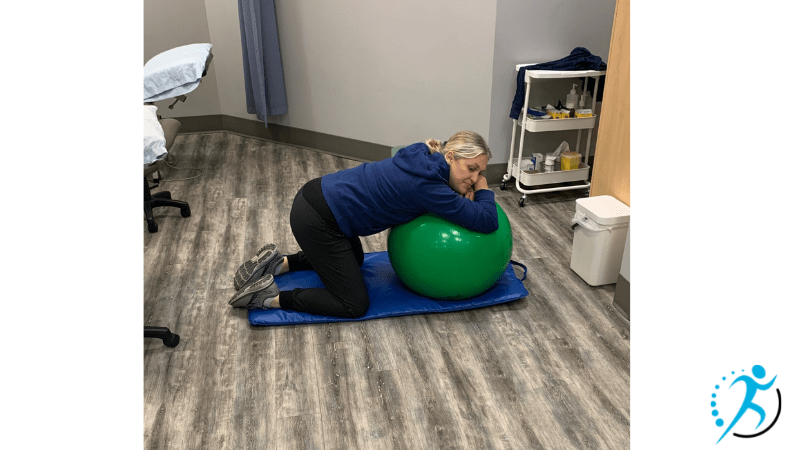
- Kneeling (using ball or top of an upright hospital bed): Similar to quadruped but the added benefit of extra support and less pressure on hands and wrists.
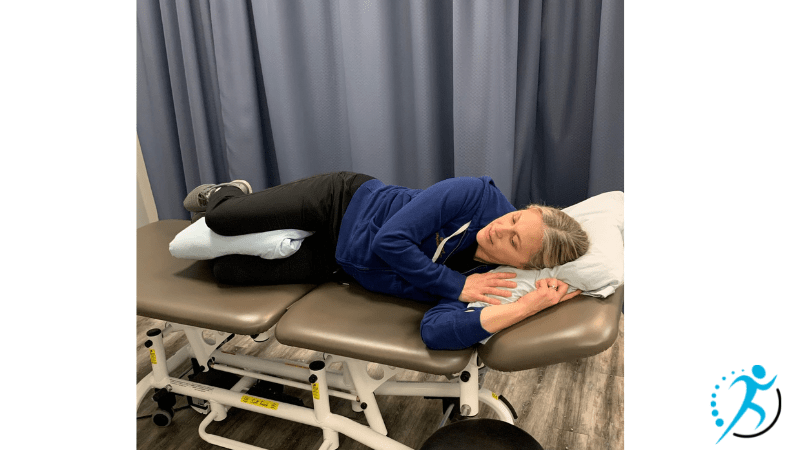
- Side lying (leg supported, peanut): Allows for rest between contractions. The sacrum is able to move freely and interventions are easy to perform in this position. A great position too if pain management is used and unable to get into upright positions. Demonstrates decreased incidence of a higher degree of tears. The leg can be supported by a partner, with a pillow or even a peanut (peanut-shaped ball with is wedged between knees for leg support)
Upright positions allow for gravity to assist the baby in descending into the birth canal and opening the pelvic outlet. Research shows that upright positions produce less severe tearing, are less likely for vacuum and forceps, decreased pushing time, and overall, improved satisfaction of the birth experience.
Of all the positions listed, Quadruped and side-lying demonstrate the best outcomes for the reduction in the severity of perineal tears.
Another important thing to discuss is pain management. Epidurals are very effective in pain management and should be offered to birthing mothers as the first line of care. Epidurals can now be low doses. So, it’s possible to still move and choose your preferred birth position, although you may need extra support from your partner. As mentioned above, a side-lying position is a great option if full upright positions are not able to be achieved.
In conclusion, it’s important to note that although these birthing positions are aimed to reduce peroneal tears, instrument intervention and improve the overall birth experience, the very nature of birth is unpredictable and if the safety of your baby or yourself is at risk, that it’s not always possible to choose our birth position. Be proactive and talk to your health care provider ahead of time about your birth plan, different scenarios and interventions. Speak up if things aren’t going as planned, if you don’t feel supported or if you need a change.
If you have an upcoming birth, I wish you and your little one the very best. Deep breaths. Trust yourself. Remember to follow up with your pelvic floor therapist 6-8 weeks post-partum to assist in your full recovery. You can do it, MAMA!!!

Written by Nicole Endicott
Nicole has been passionate about medicine and movement her entire life. Her treatment philosophy is based on patient education, manual therapy, IMS and individualized exercise prescription. Her clientele ranges from children to seniors, with a special interest in women’s health prenatal & postpartum populations. She also is well versed in sports injuries, motor vehicle rehabilitation and assisting people in their active lifestyle. Nicole is a lifelong learner and continues to take many classes in the advanced orthopaedic manual and manipulative therapy division and in women’s health. She is kind, compassionate and eager to assist in reaching your movement and activity goals.
References:
- Badillo, V. Bobb, S. Gallagher, K. Lithos. S. Steffes, R. Stephenson, J. Quinonez. Section of Women’s Health, American Physical Therapy Association. 2014, pages 330-345.
- Labour and Delivery. My Health.alberta.ca. October 8, 2020. https://myhealth.alberta.ca/Health/Pages/conditions.aspx?hwid=tn9759
- Priddis, H. Dahlen, V. Schmied. What are the facilitators, inhibitors, and implications of birth positioning? A review of the literature. Women and Birth. Volume 25, Issue 3, September 2012, pages 100-106.


