
Not all leg pain is sciatica: The evolution of deep gluteal syndrome
Do you have pain in your buttock region, hip, thigh or back of the knee? Are you puzzled about what is causing this because you don’t remember injuring yourself? Is the pain keeping you up at night? Have you been told by your family doctor, a family member, or a friend that you have sciatica or sciatic nerve pain? You are not alone! Buttock and leg pain is very common and is experienced by up to 14% of the population. However, it cannot always be attributed to Sciatica.
What is sciatica?
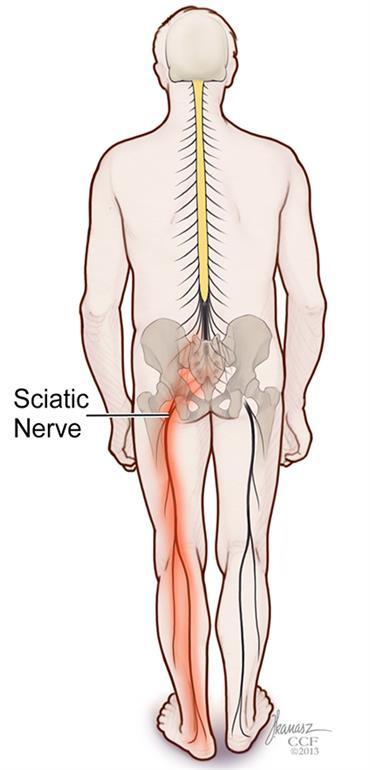
Sciatica aka piriformis syndrome were terms previously used to describe any condition which involves pressure or damage to the sciatic nerve. The sciatic nerve is a large nerve that runs down the back of your leg, carrying the electrical signals to your upper/lower leg and foot. These electrical signals are responsible for your sensation and creating leg movement. When the sciatic nerve is compressed or injured it can cause pain, tingling or numbness from the back of the thigh to the knee and occasionally the foot. Additionally, compression or injury to the sciatic nerve can cause weakness in the leg muscles.
Traditionally, a muscle called the piriformis was the proposed culprit for this ‘sciatic’ pain. Dysfunction of the piriformis can place tension on the sciatic nerve resulting in this pain or sensory experience. However, the piriformis is not always the cause of this pain. There are many other joints, muscles and connective tissues that are in the same location and may be at fault.
Picture of piriformis muscle
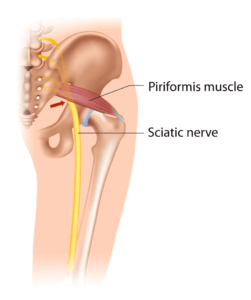
As seen in this image, there any many muscles, ligaments, and nerves in the back of the hip. The image in yellow is the sciatic nerve. You can see that there are many branches of this nerve.
Out with the old, in with the new:
The term deep gluteal syndrome is now commonly being used in place of piriformis syndrome and sciatica. Deep gluteal syndrome is an overarching term that is used to describe a cluster of conditions that can cause similar symptoms, mostly resulting in pain in the back of the hip/buttock and down the leg. These conditions include sciatica, Ishiofemoral impingement, pudendal neuralgia, or a hamstring tendinopathy. These terms may seem complex and intimidating, but they all result in relatively the same symptoms and are managed similarly.
What symptoms might I experience with deep gluteal syndrome?
You may have one or more of the following symptoms if you are experiencing deep gluteal syndrome:
– A deep, achy pain that may be felt in the back of the hip all the way down to the knee. It is usually one sided.
– Tingling or numbness down the back of leg, down to the knee and occasionally to the foot
– Pain that is worse with walking, running, stairs, lifting, standing, or sitting for prolonged periods of time
– Pain that is worse at night
– Mild weakness in the muscles around the hip
– A catching or locking sensation felt in the back of the hip
Who experiences deep gluteal syndrome?
– Patients who have had previous injury or surgery to their hip or buttock region
– Patients who are sedentary
– Patients who have given birth
– Patients who are over-weight
How do I get rid of this pain in the butt?
As deep gluteal syndrome can be caused by multiple factors, it is best to be evaluated by a physiotherapist.
At Avenue Physio, a physiotherapist will be able to:
1. Conduct a physical examination to rule out other serious pathologies
2. Perform hands-on treatment and use evidence informed modalities
3. Provide you with a home exercise program to help decrease your pain and speed up your recovery.
4. Help you pace your athletic recreational activities and give you ergonomic advice
What can you do for yourself?
While waiting to see a physiotherapist there are some actions you can take to help manage your pain:
If you do not currently exercise, start trying to increase your activity level by going for 15-30 minute walks, 1-2 times per day
2. Take breaks at work, stand up and walk around for at least 1-5 minutes every hour
3. Use a 0-10 pain scale to pace your physical activity:
– Pain should NOT increase more than 3 points during exercise
– Pain should return to pre-exercise levels within an hour of stopping
– There should be no increase in stiffness or pain the next day
** If you experience any of the above 3, you should reduce the amount or intensity of your exercise **
4. Some examples of ways to pace your current physical activity include:
a. Add 30 seconds/km to your run pace or break your activity up into shorter times
b. Take shorter strides while running
c. Reduce the weight you are lifting at the gym, increase repetitions slowly
d. Warm-up prior to any activity
5. Move your car seat slightly closer to the steering wheel, this will reduce strain on the sciatic nerve and hamstrings
FAQ’S
What does Sciatica feel like?
Sciatica typically occurs on one side of the body. The sciatic nerve is the largest nerve in the body and is formed by the union of 5 nerve roots from the lower spine. The pain from this nerve is unique and is often described as shooting, searing pain that is felt in the buttocks and radiates down the leg. It can be accompanied by the sensation of numbness, tingling or burning. It is important to note that not all leg pain is from the sciatic nerve. It must be accompanied by these qualities to be the nerve.
How common is deep gluteal syndrome?
This condition is rare. It affects less that 1% of the general population. For patients who present with sciatic pain only 6-8% is due to irritation in the deep gluteal region.
Is walking good for piriformis syndrome?
It is important to keep moving when you have a flare up of pain. Aerobic exercises are important for you hip muscles and overall health. Walking can be a good exercise to keep you moving. However, if the nerve is sensitive it will not like to be stretched as in
taking a stride. You may need to decrease the length of your stride by taking shorted steps and walking slower to not irritate your symptoms.

