
How To Relieve Your Low Back Pain
So here’s a story almost everyone has heard: “I was bending over putting on my socks when all of a sudden my back seized up on me!” Or “I was bending over to pick something off the floor when I had to cough. I had this sharp pain and I couldn’t stand up straight for a week!”
Lower back pain affects 75% of the population at some point in their lifetime. Besides the common cold, lower back pain is the most common complaint for family physicians, and for physiotherapists low, back pain is THE most common complaint!
Thankfully, almost everyone who experiences low back pain will have almost total relief within about 6 weeks. The real problem is when the low back pain strikes again…and again…and again.

Symptoms of Low Back Pain
Depending on the underlying cause of the pain, symptoms can be experienced in a variety of ways. For example:
- Pain can range from a dull ache to stabbing or shooting in sensation
- Other sensations may include numbness or tingling in the leg
- Muscle spasms and tightness in the low back, pelvis, and hips
- Pain can be isolated to one side of your low back or both sides, it can spread into your buttocks or refer down your leg
- Pain that worsens after prolonged sitting or standing
- Symptoms can be mechanical which means it occurs with certain movements like getting up from sitting, forward bending, and standing up straight
How Long Should my Lower Back Pain Last?
This is always an interesting question because there really isn’t a simple answer. Tissue healing generally occurs within weeks, so in optimal conditions, recovery should be fairly quick. (It’s never as quick as we’d like, but most people would accept 6-8 weeks over 1-2 years, so the perspective is key!)
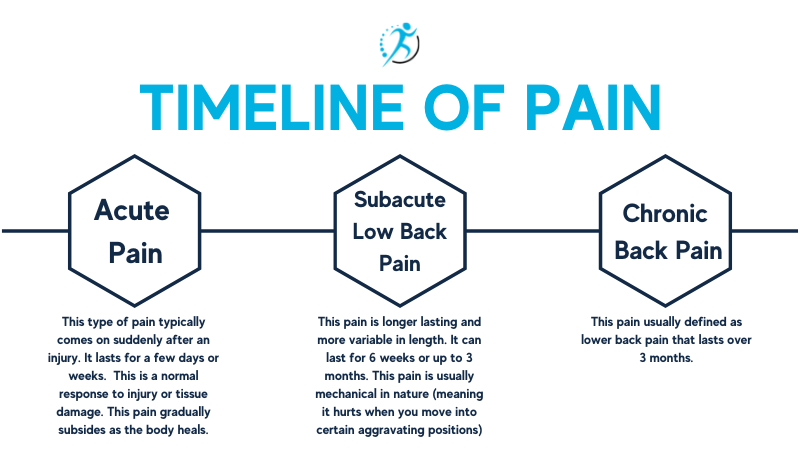
About 20% of people who experience acute lower back pain progress on to have persistent back pain that lasts greater than 1 year.
What Causes Lower Back Pain?
Sprains & strains – this means aggravation or injury to the muscles, ligaments, joints, and occasionally the discs
Sciatica – injury to the nerve that runs down the back of your leg most likely the cause of a disc protrusion
Pelvis injuries – the Sacro-iliac joint can be injured by trauma or during or after pregnancy
Arthritis –osteoarthritis or autoimmune diseases
There are more sinister causes of lower back pain, the ones nobody wants to talk about. Tumors, Cancer, Infections, Blocked arteries, and kidney stones can all cause significant lower back pain as well, which is why when faced with an episode of low back pain it’s always best to consult either your physician or your physiotherapist. Thankfully, these are extremely rare, and the path to recovery can start right away.
How Can Physiotherapy Help?
Physiotherapists have an excellent understanding of back pain. We will start by taking a thorough history and doing a clinical exam which helps to determine what is causing your lower back pain in the first place. This is followed by education about what to expect, how to modify your activity to speed up your recovery, exercises to regain mobility and strength around your spine, and either hands-on treatment, acupuncture, and/or electrical modalities to assist with pain management. Most likely, your physiotherapist will be in contact with your doctor so your medical team can take a multi-modal approach so that your recovery can be as fast and complete as possible.

How Can I Help Myself?
There are many different ways we can either prevent back pain from occurring or re-occurring.
First – Maintain an active lifestyle. Whether you have pain or not, it’s important to stay active. A sedentary lifestyle leads to muscle imbalances, weakness, poor posture, obesity, and poorer coping mechanisms.
Recommendations:
- 150 minutes per week of moderate exercise. This can include walking, swimming biking. Anything that you like to get you “huffing” and “puffing” a bit.
- Muscle-strengthening activities at a moderate intensity involve all muscle groups 2 or more days a week. This can include golfing, Pilates, weight lifting, and tennis. Anything that gets your big muscles working against some resistance, even gravity!
Research shows that a strong core (both stomach muscles AND back muscles) will help to reduce occurrences and recurrences of lower back pain. So it’s very important to stay strong.
Second – Almost as important as the first! is to maintain a positive outlook! While this may seem far-fetched, people who perceive that they are in control of their lives have a much better prognosis than people who believe that some outside force is responsible for their pain!
Another key point in helping yourself is to seek professional advice early in the process of dealing with your lower back pain. Early intervention has been shown to drastically improve outcomes in a shorter period of time. Take care of yourself, you are important!
I am in pain now What should I do?
Stay calm – remind yourself that low back pain is very common and rarely dangerous. Most episodes of low back pain improve.
Modify your movement – Rest from any aggravating activity. Avoid prolonged sitting, driving, bending, heavy lifting, and twisting.
Early exercise – Do gentle exercises for mobility and stretching.
Keep moving – keep walking and puttering about. Depending on your pain levels you may have to modify your movement but don’t stop everything and lay in bed.
Positioning – Modify your sleeping position to ease the strain on your low back. Make sure your bed is firm enough to give you adequate support. If you sleep on your back, try putting a pillow under your knees. Or if you prefer to sleep side-lying, put a pillow between your knees and a folded towel under your waistline.
Imaging – Don’t think that you need imaging like an x-ray or MRI to “find” out what is wrong. Rarely is imaging required to treat low back pain. There are very specific symptoms and signs that are assessed that then require more investigation with imaging.
Try ice and heat – you may have heard that one is better than the other for relief from back pain. The short answer is that the best option is whichever works for you. Usually, ice is best if you have inflammation and a heating pad may be better if you are feeling stiff and tight.
Over-the-counter medication Discuss options with your pharmacist – Non-prescription pain relievers like NSAIDs and acetaminophen can be helpful for managing inflammation and pain.
Seek the advice of a physiotherapist if you have questions or the pain persists for greater than a week or is worsening you should seek the advice of a physiotherapist.
Back Pain can be short-term or long-term, it can be simple or complex, and it will affect almost all of us at some point in our lifetime. By taking a team approach including your physiotherapist, physician, and most importantly yourself, you can limit the consequences of a back injury and stay functional and pain-free.
The physiotherapists at Avenue Physio are experienced in managing both acute and chronic low back pain. So the next time you experience low back pain give Avenue Physio a call and we will get you back to doing the things you love.
Want to learn more? check out our GLA:D BACK PAIN PROGRAM
https://avenuephysio.ca/glad-back-pain-program/
FAQ’S
What is the most common cause of low back pain?
The most common cause of low back pain is muscle and tendon strains and ligament sprains. Muscle strains can happen suddenly when you lift something too heavy or awkwardly. Or pain can develop slowly over time from repetitive movements.
Is it better to sit or lay down with low back pain?
You should find a position that relieves the pain. Usually laying down with a pillow under your knees provides more relief because it ‘unloads’ your back and you can relax your muscles. The goal should be to regain your ability to move by walking first then work on your ability to sit in one position.
How do I know if my low back pain is serious?
More serious causes of low back pain are rare. But there are more sinister reasons for low back pain that may require medical assessment and intervention. Symptoms that we call “red flags” that may require investigation by your physician, or your physiotherapist are:
- Problems with your bowel or bladder
- Pain that is worsening
- Unremitting pain that is disturbing your sleep
- Numbness, weakness, or tingling in your legs
- Unexplained weight loss
- Fever
- Intense localized pain and an inability to get into a comfortable position

Written by Kelly Barrie
Kelly is the owner of Avenue Physio and is proud to be part of a supportive and personable team that is dedicated to providing a high quality of treatment and experience to patients. She has been a physiotherapist for over 25 years treating a range of orthopedic conditions including chronic pain, motor vehicle collisions, and sports injuries (from the weekend warrior to high level). Kelly has always been passionate about movement and promoting healthy lifestyles. First, as a Certified Personal Trainer, and for the last 25 years as a physiotherapist. Kelly has completed the highest level of Certification in Manual and Manipulative Therapy that is internationally recognized (FCAMPT). Advanced knowledge of strengthening programs, manual therapy skills, and critical thinking optimize her treatment plans for her patients so they can reach their movement goals.
