Ur-ine Control of Your Bladder
Are you tired of leaking urine with certain activities? Are you fed up with leaking urine while constantly running to the washroom?
Well you are not alone….
Urinary incontinence affects 3.3 million Canadians!
What is urinary incontinence?
- Urinary incontinence is the involuntary (meaning you cannot control it) leakage of urine.
As we age, leaking urine is normal, right?
According to The Canadian Continence Foundation (2018), “No! The changes that occur as we get older (like menopause in women or prostate enlargement in men) may contribute to incontinence, but that doesn’t mean you just have to live with it. Almost all cases of urinary incontinence can be treated, managed, or cured.”
The main types of urinary incontinence that woman experience:
- Stress Urinary Incontinence: leakage of urine when you cough, sneeze, laugh, exercise, or lift objects.
- Urge Urinary Incontinence: occurs when you have an urgent need (get out of my way!) to urinate, and you are unable to make it to the toilet in time.
- Often women have urinary triggers (situations that make you have to go!):
- Running water
- Cold temperatures
- Arriving at home, placing your key in the door
- Often women have urinary triggers (situations that make you have to go!):
- Overactive Bladder: may have the strong urge to urinate but may not leak urine. Also experience frequent trips to the washroom.
- Mixed Urinary Incontinence: having both stress and urge urinary incontinence.
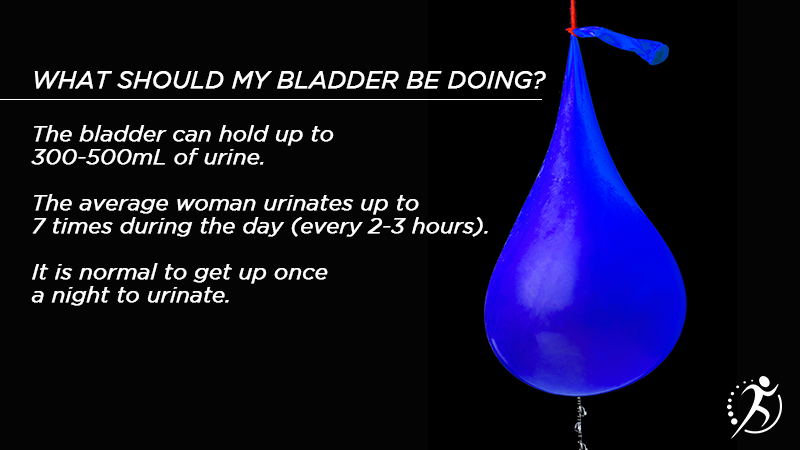
What is the bladder and how does it work?
But WHY do I have urinary leakage?
- Pregnancy/vaginal delivery
- Aging
- Bladder Pain Syndromes
- Constipation
- Medicine
- Surgery
- Bladder cancer or stones
- Menopause
- Overweight
- Smoking
- Chronic cough
What can I do to treat my urinary incontinence?
1. Lifestyle Changes
- Drinking 6-8 cups of fluid (water) per day
- Avoiding caffeine, alcohol, and carbonated drinks (cause irritation to the bladder)
- Drinking less than 6-8 cups of water per day can make the urine concentrated which can also irritate the bladder.
- Avoiding constipation
- Repetitive straining can cause damage to the pelvic floor muscles, supportive tissues, and pelvic floor nerves.
- Places pressure on the bladder and urethra which can lead to increased trips to the washroom or unable to fully empty the bladder.
- Achieving a Healthy Weight
- Nutrition
- Exercise
2. Pelvic Floor Muscle Training
- How do I find the pelvic floor muscles?
- Imaging that you are trying to stop the flow of urine
- Imaging that you are trying to stop the passage of gas
- Imaging that you are trying to lift a marble at the vaginal entrance up and in.

What if I still do not know if I am doing it right?
- You can take a mirror and look. You should see your vaginal entrance and your anus draw up and in. That is a pelvic floor contraction, or “Kegel”
- OR you can insert your clean finger into your vagina, you should feel like your finger is being drawn up and in.
What if I STILL do not know if I am doing it right?
- You may need guidance from a pelvic floor physical therapist.
How do I strengthen my pelvic floor muscles?
Pelvic Floor Muscle Training, “Kegel”
- Start by laying down with your knees bent
- Contract (squeeze) the pelvic floor muscles:
- Hold for 5-10 seconds
- Relax for 10 seconds (important to relax the pelvic floor muscles!)
- Repeat: 5-10 times
- Complete 1-2 times a day
The Knack
- Contract (squeeze) your pelvic floor muscles before you cough, laugh, sneeze, or lift. *Useful for stress urinary incontinence*
To Kegel, or Not to Kegel: that is the question
- “Kegels” or pelvic floor muscle contractions are sometimes not always the answer!
- Some women may have tight pelvic floor muscles and the “Kegel” or pelvic floor muscle contractions may not solve their problems!
- https://youtu.be/YW-9UUumQgw
3. Bladder Retraining
- Learning how to control the bladder muscles
- When you feel the urge to urinate (the I have to go sensation):
- Be still
- Sit down. Can cross your legs. Or stand with your legs crossed and bend over like you are trying to tie your shoes.
- Complete pelvic floor muscle contractions.
- Take a few deep breaths and relax
- Distract your mind (keep on going with your task, count, etc.)
- When the urgency disappears, then you can calmly walk to the washroom.
* Useful for overactive bladder, urge urinary incontinence, and mixed urinary incontinence*
What is Pelvic Floor Physiotherapy?
- Rehabilitation of your pelvic floor that will include:
- Education, exercises, strategies, and techniques to help manage, prevent, and treat your symptoms.
- Pelvic health physiotherapists are physiotherapists who have completed specialized training to assess and treat pelvic floor dysfunctions.
- Assessment begins with a thorough review of your medical history, questions about your drinking, eating, voiding, and sexual habits as it relates to your symptoms.
- Followed by an assessment of your posture, hips, abdominal and pelvic floor muscles for tightness, weakness, and/or strain.
- This may include a pelvic floor exam.
Why do you complete an internal pelvic floor exam?
- To assess your pelvic floor function and to tailor an exercise program that will help you meet your goals.
- Review if you can complete pelvic floor muscle exercises correctly. Many women require the help from a pelvic floor physiotherapist to ensure that they are engaging the appropriate muscles.
- Tight pelvic floor muscles will not respond well to pelvic floor strengthening exercises, or “Kegels”. Assessing the pelvic floor will help guide the appropriate exercises for you to be given.
View this post on Instagram
Written by Kayla Skjerdal, Pelvic Physiotherapist
Kayla has experience working with patients with a range of orthopedic concerns including motor vehicle injuries, worker-related injuries, sports injuries, post-fractures, post-surgical, bursitis, tendinitis, muscle sprain/strain, muscle tears, and women’s pelvic health concerns. Kayla is always taking courses every year to stay up to date with the research so that she can provide her patients with the best care possible. Kayla uses a variety of treatment tools such as manual therapy, dry needling, exercises prescription, and education to help her patients reach their rehabilitation goals.
Kayla has a passion for treating women’s pelvic health concerns. She has taken many courses to help treat many pelvic floor dysfunctions such as urinary and fecal incontinence, pelvic organ prolapse, pelvic pain, pain with intercourse, and pre and post-partum concerns. She loves empowering women to gain control of their bodies, improve their quality of life, and get back to their activities.
Resources:
- The Canadian Continence Foundation. (2018). The Source: Your Guide to Better Bladder Control. 2018. https://www.canadiancontinence.ca/EN/the-source-guide.php
- Pelvic Health Solutions. (2021). Constipation. https://pelvichealthsolutions.ca/for-the-patient/constipation/
- Saskatchewan Pelvic Floor Pathway. (2018). Information for Woman About Incontinence & Vaginal Prolapse. http://www.sasksurgery.ca/pdf/pelvic-floor-booklet.pdf

