
BUILDING STRONGER GLUTE MUSCLES TO HELP PREVENT RUNNING INJURIES
After having my daughter finding time to be active became a challenge. The easiest solution … hop on the treadmill during nap time. Power off as many kilometres as I could before she woke up. Lace-up and repeat the next day. But I was neglecting a key component. STRENGTH. I soon began to get a bit achy … the knees and hip let me know they weren’t a fan.
Does this sound familiar? Or do you notice that as your mileage increases you start to get aches and pains? Is muscle fatigue and/or pain affecting your ability to run long distances? If so you are not alone. Running is one of the most popular forms of exercise in the world. But up to 50% of all runners will sustain an injury that will affect their ability to run or their performance.

But, if you increase your activity levels too quickly, you may sustain an injury that will put you right back where you started.
So, if you are restarting an activity or starting a new one, be sure to make injury prevention a priority so that you can continue to participate in the long term.
Before we talk about how to avoid injury, first consider:
What are the common injuries related to running?
The injuries most commonly reported related to running are:
Patellofemoral pain syndrome:
- An umbrella term used to describe pain around the patellofemoral joint (your knee cap and thigh bone)
- Usually results in pain on the front of the knee
- Usually related to overuse and overload of the patellofemoral joint
- Often underlying muscle weakness is a contributing factor
Iliotibial (IT) band friction syndrome:
- Compression of structures on the outside of the knee from tension generated in the IT band
- A non-traumatic overuse injury
- Pain around the outside of your knee
- Weakness in the hip abductor muscles through to play a large role
Plantar fasciitis (10% of all running-related injuries)
- The most common cause of heel pain
- An overuse injury that is primarily due to repetitive strain causing micro-tears in the fascia on the bottom of the foot
Patellar tendinopathy
- Pain located at the bottom of the knee cap
- Pain is made worse with increased load and increasing demand of the knee extensor muscles
Do you see a theme with these common running-related injuries is? Overuse.
Some of the strategies that can be used to prevent or lessen the likelihood of an overuse injury include:
- Cross-training
- Progressively increasing training load
- Preparing your body to manage increased load … Strengthen!

What muscles are active during running
There are two main phases you go through when you run. Stance and swing (these make up your gait cycle)
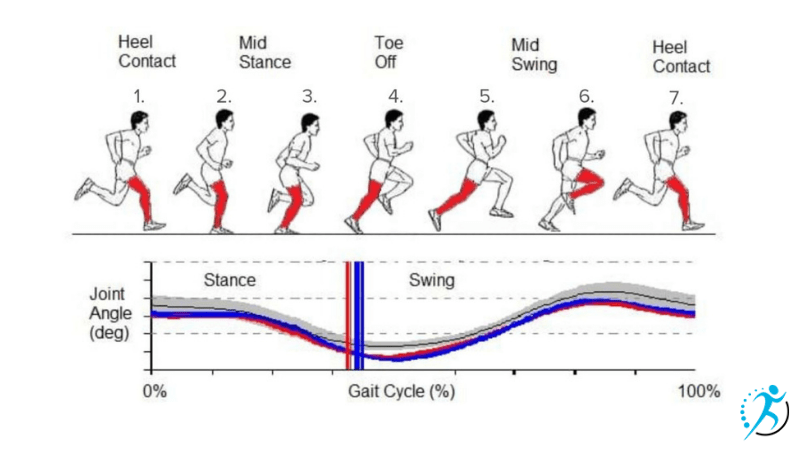
Stance Phase: from when your foot strikes the ground to when you push off
Swing Phase: when the foot is not in contact with the ground
When it comes to injury prevention the stance phase is what we tend to focus on. It makes up about 40% of the total gait cycle. It is also when your foot and leg are supporting your body weight.
What Muscles are used During the stance phase
Of all the muscles in your leg, studies have shown that the gluteal muscles are the group that is the most active during the stance phase. That’s right, your butt muscles are working hard to give you a stable base to work off and propel you forward.
The gluteal muscle group is made up of the following three muscles: Gluteus Maximus, Gluteus Medius, and Gluteus Minimus.
Here is some more information on each of these muscles, along with some of the best exercises to get them working and build strength.
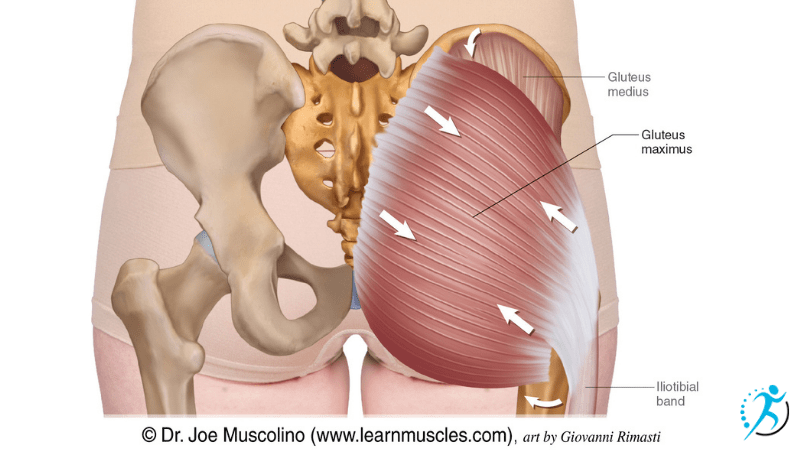
Gluteus Maximus
Location
- located on the back of the hip
- originates along the hip bone and sacrum and attaches to the greater trochanter and the Iliotibial band
Action
- Extends the hip
- Externally rotates the hip (turns it outward)
Activity during the stance phase of running (peak muscle force): 15.8 N/kg
(a measure of peak muscle force via EMG study)
Exercises that target Gluteus Maximus
single-leg glute bridge
- laying on your back with your arms at your side, lift one leg off the floor slightly
- as you push into your foot, lift your butt off the ground keep your pelvis level (don’t let it dip side to side)
- Hold for 5-10 seconds (without sacrificing form) and slowly lower back down
- Repeat
Donkey kick with bands
- start on your hands and knees
- wrap a band around your foot and hold it with the opposite hand
- maintain a neutral spine position as you kickback
- keeping the knee bent will decrease the role of the hamstrings during this exercise
Step-ups
- Start with a step that comes midway up your lower leg, if the exercise is too easy you can choose a higher step
- Place a foot on the step and step up so both feet are on the step before coming back down
- You should focus on bending more at the hips than the knee. If most of the movement comes from the knee you will be using your quadriceps more than your glutes.
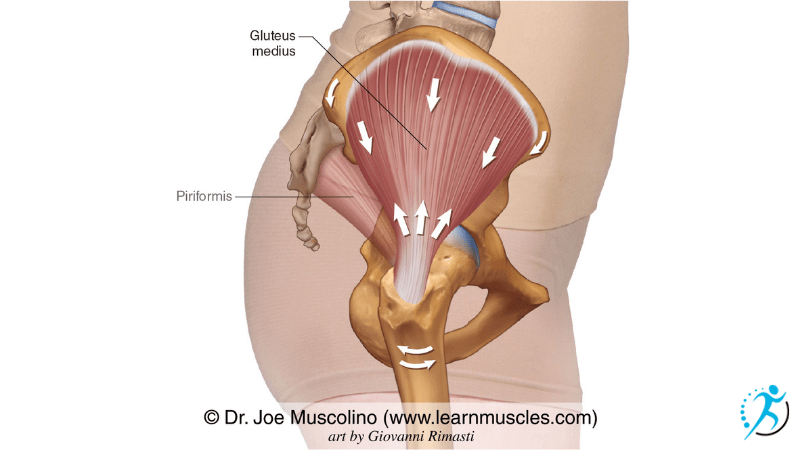
Gluteus Medius
Locations
- on the outside of the body
- extends from the top of the pelvis (iliac crest) across the hip joint to the top of the femur (on the greater trochanter)
Action
- moves your leg out to the side (abduction)
- stabilizes the hip during single-leg stance, keeping the pelvis from dropping
Activity during the stance phase of running: 32.05N/kg
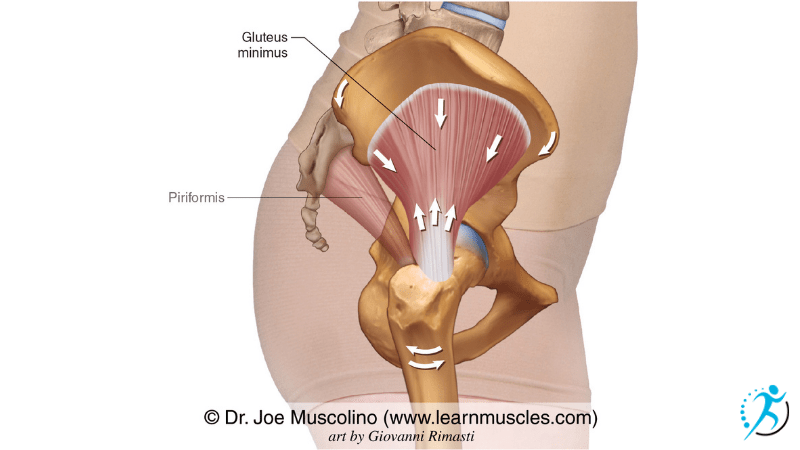
Gluteus Minimus
Location
- located underneath the gluteus medius muscle
Action
- assists the gluteus medius with abduction
- stabilization of the hip during single-leg stance
Activity during the stance phase of running: 22.97 N/kg
Exercises that target the gluteus medius and gluteus minimus
Side-lying abduction
- lay on the ground with your bottom leg bent up
- think about tipping your belly button towards the ground at about a 45-degree angle and keep it pointed here during the exercise (this cue just helps ensure that you won’t rotate back).
- As you lift the top leg up, you should think about keeping the shoulder, hip, knee, and ankle in a straight line.
Banded walking
- Place a looped band, or tie a theraband, around your feet. There should be a fair amount of tension in the band just standing with feet hip-width apart.
- in a slight squat position take a large step forward and to the side, repeat with the other side
Sidewall sit/squat
- Stand beside a wall with both feet hip-width apart, the foot that is closest to the wall should be 2-3 inches from the wall
- Place your leg closest to the wall against the wall, with the foot a couple of inches off the ground and the knee and hip bent
- Push the knee into the wall as you squat down slightly
- Hold
- The goal would be to hold this for up to 5 minutes
So the next time you have a running injury or if you’re just not meeting your running goals give us a call at Avenue Physio. I would love to help you meet your goals of running pain-free and preventing injuries.

Written by Jenna Armstrong
Jenna was born and raised on a farm outside of Killarney, Manitoba, and moved to Alberta in 2005. She obtained her Bachelor of Kinesiology with Distinction from the University of Calgary and a Master’s of Science in Physical Therapy from the University of Alberta. Jenna also attained a Personal Training designation with the Canadian Society of Exercise Physiology.
During her career, Jenna has made continuing education and skill development a priority. She completed her Integrative Dry Needling certification as well as the Gunn Intramuscular Stimulation (IMS) certification at the University of British Columbia. Jenna has successfully completed her Diploma of Manual and Manipulative Physiotherapy and is a fellow with the Canadian Academy of Manipulative Physiotherapy. Additionally, she has taken courses in diagnostic imaging and treatment of the myofascial system. She strives to incorporate information from the courses she has taken and the latest research into her treatment and uses a wide variety of treatment techniques. This includes education, dry needling, joint mobilization and manipulations, neural tissue mobilization, soft tissue techniques, and exercise prescription.
References:
- Buchanan BK, Kushner D. Plantar Fasciitis. [Updated 2021 Jul 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-.Available from: https://www.ncbi.nlm.nih.gov/books/NBK431073/
- Dack, D. (2017, June 10). The running gait cycle explained. https://www.runnersblueprint.com/running-gait-cycle/
- Fairclough J, Hayashi K, Toumi H, Lyons K, Bydder G, Phillips N, Best TM, Benjamin M. The functional anatomy of the iliotibial band during flexion and extension of the knee: implications for understanding iliotibial band syndrome. Journal of Anatomy, 2006; 208(3): 309-316
- Juhn M. S. (1999). Patellofemoral pain syndrome: a review and guidelines for treatment.American family physician, 60(7), 2012–2022.
- Lenhart, R., Thelen, D., & Heiderscheit, B. (2014). Hip muscle loads during running at various step rates.The Journal of orthopaedic and sports physical therapy, 44(10), 766–A4. https://doi.org/10.2519/jospt.2014.5575
- Malliaras P, Cook J, Purdam C, Rio E. Patellar Tendinopathy: Clinical Diagnosis, Load Management, and Advice for Challenging Case Presentations. The Journal of orthopaedic and sports physical therapy. 2015 Sep:1-33.
- Nielsen, R. O., Nohr, E. A., Rasmussen, S., & Sørensen, H. (2013). Classifying running-related injuries based upon etiology, with emphasis on volume and pace. International journal of sports physical therapy, 8(2), 172–179.
- Van Gent RN, Siem D, van Middelkoop M, van Os AG, Bierma-Zeinstra SMA, Koes BW. Incidence and determinants of lower extremity running injuries in long-distance runners: a systematic review. Br J Sports Med. 2007;41(8):469–80; discussion 480.
